Somewhere along the line, in the months and months of adoption paperwork, you have to fill out a medical needs checklist. It’s sort of an odd task because if I had given birth to a biological baby, we wouldn’t have had that list in front of us. Out she’d come and we’d love her just the same. So, it’s sort of an awkward step in the adoption process. And an awkward step in surrendering any preconceived ideas about your “healthy” baby.
Jesse and I did a lot of Googling and praying and we checked a lot of different boxes of special needs we felt God had equipped us for and lead us to.
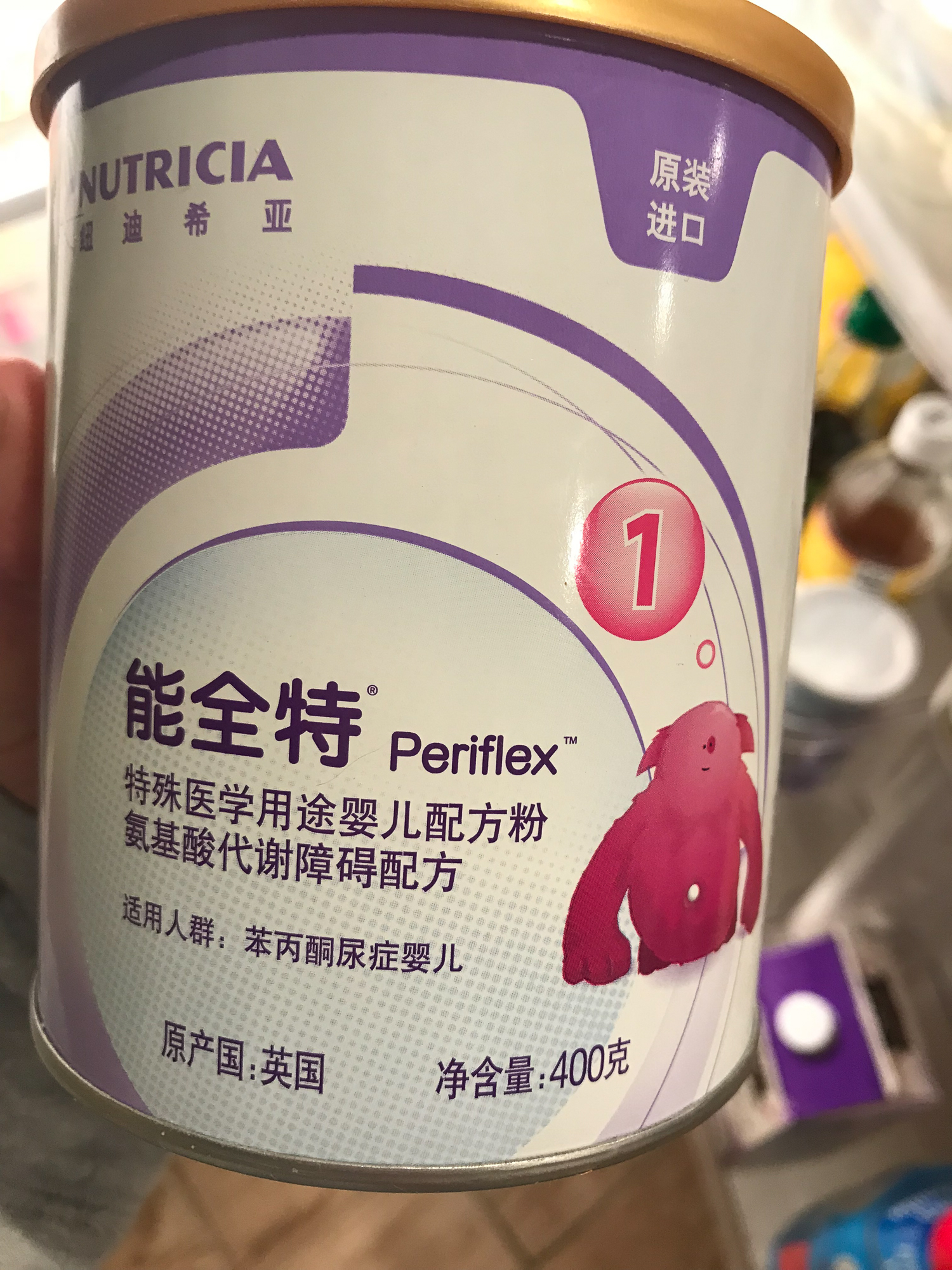
When we got The Call about Vera, the agency said something along the lines of, “We know you didn’t check that box but we wanted to call because you’ve been waiting so long and she’s so young…she has a metabolic disorder called PKU…”
That was the first time we had ever heard about PKU.
We had the agency on speaker and Jesse started researching while we were still on the phone. We scanned medical sites as quickly as we could.
Phenylketonuria. Very rare birth defect. Metabolic disorder. Causes the amino acid phenylalanine to build up in the body. When left untreated, it affects the brain. Mood swings. Behavior issues. Developmental delays. Learning disabilities. Must be on special very low protein/low Phe diet for life.
We soaked up as much as we could and told the agency very enthusiastically that YES! we’d like to see her file. While we anxiously waited and checked our inboxes 19 times a day for answers from Vera’s orphanage and lab reports to be translated, we talked to doctors and specialists to learn as much as we could. It was important to know as much as we could to prepare and have realistic expectations. We knew she was diagnosed and started taking a special medical formula very young, as far as adopted kids go (I sobbed tears of joy when I got that email), but there were/are gaps in her records. One specialist told us she was a “high risk child” because we didn’t have the numbers or photos or videos of her walking or talking to give us confidence otherwise.
High risk or not, God was telling us, “SHE IS YOUR BABY.”
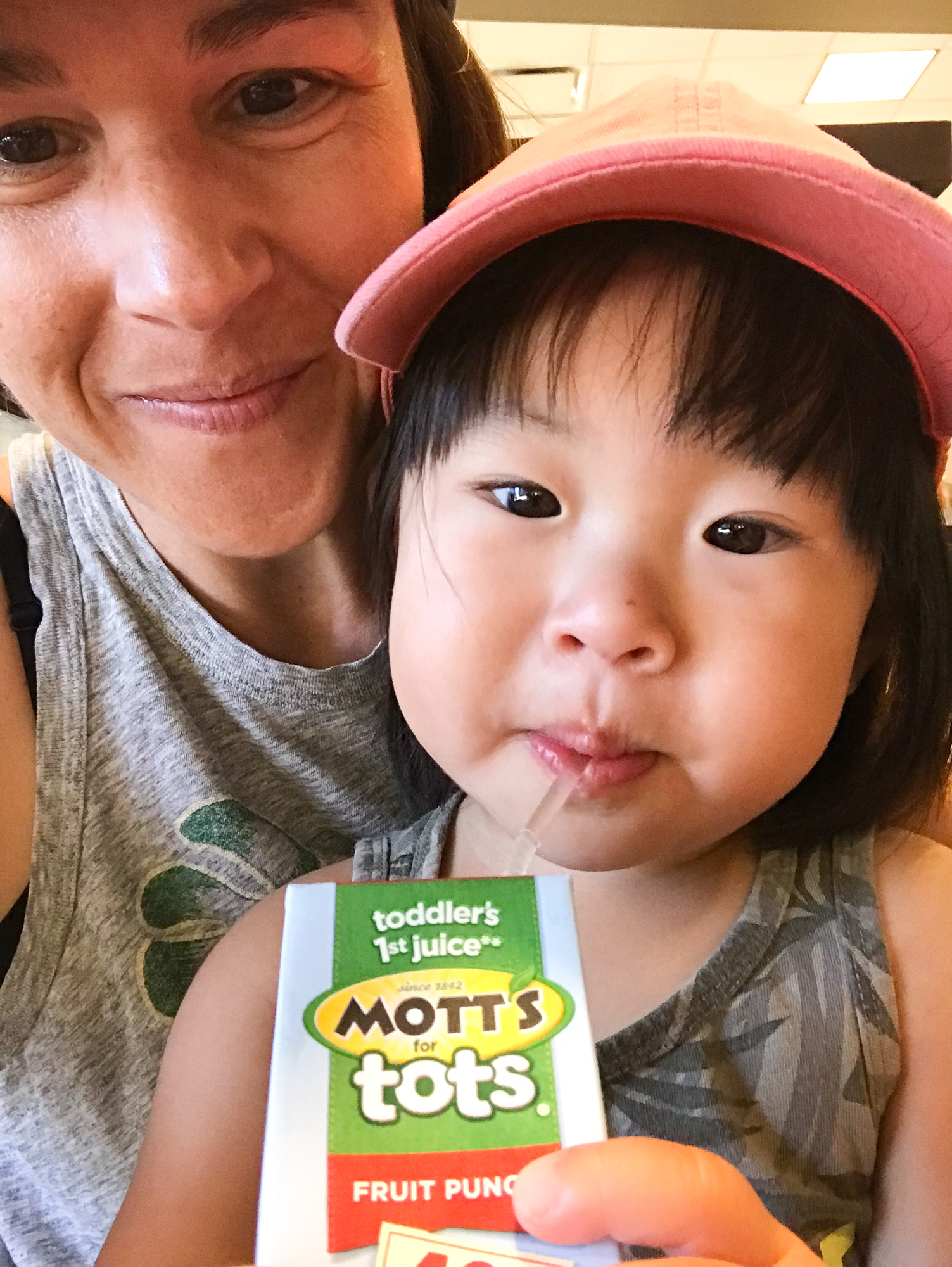
Obviously, you know by now that YES, she is our baby 😉
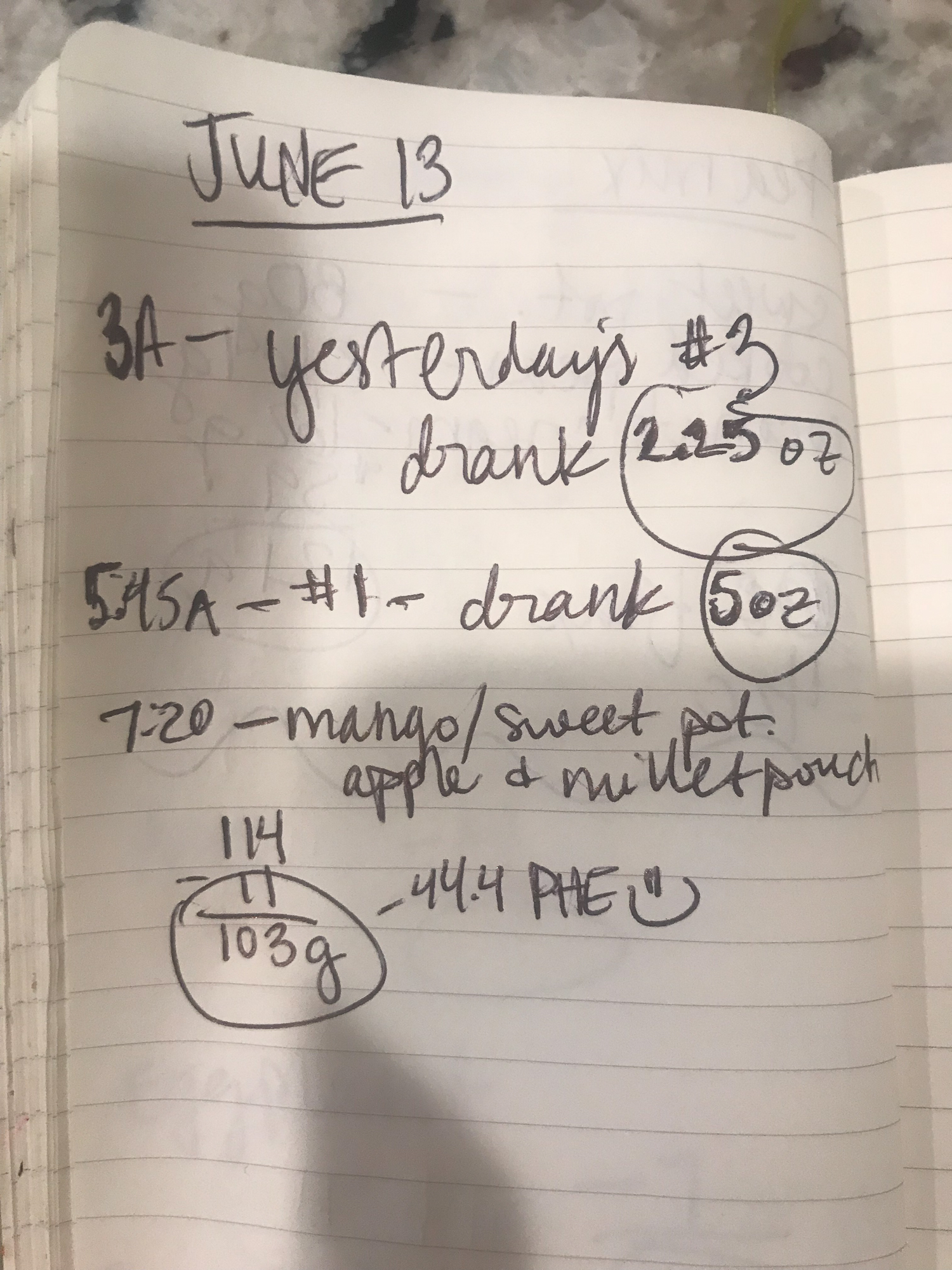
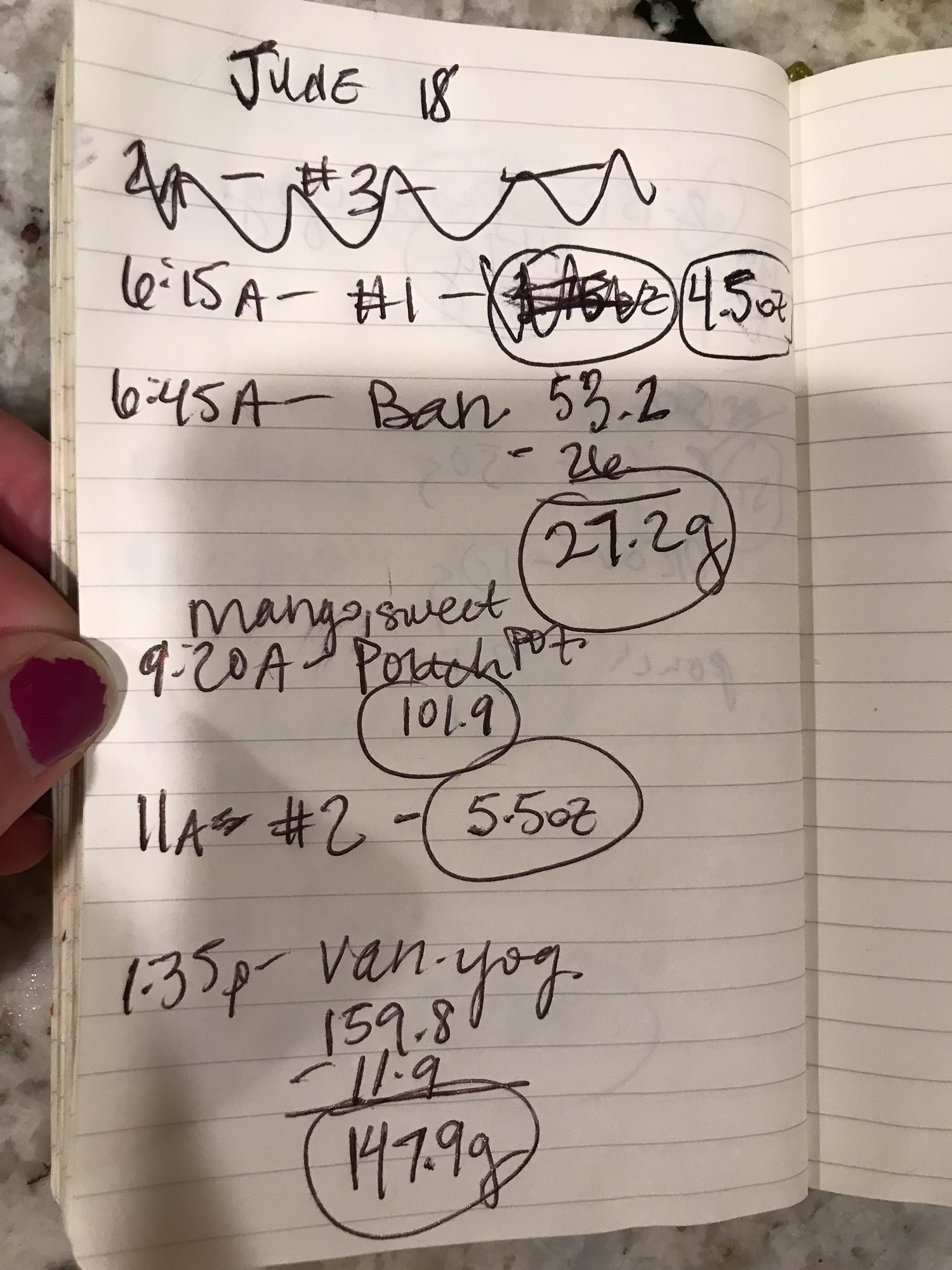
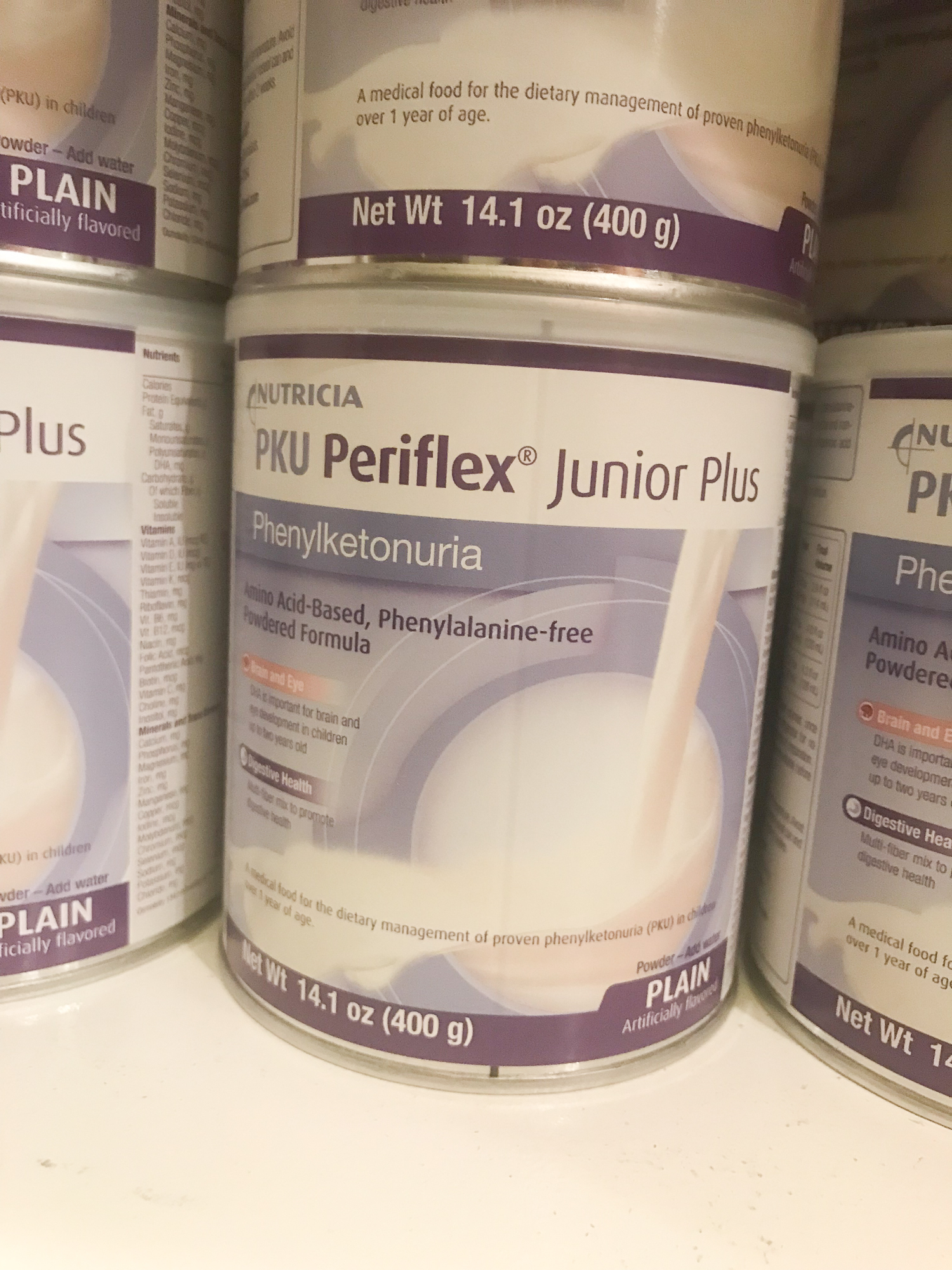
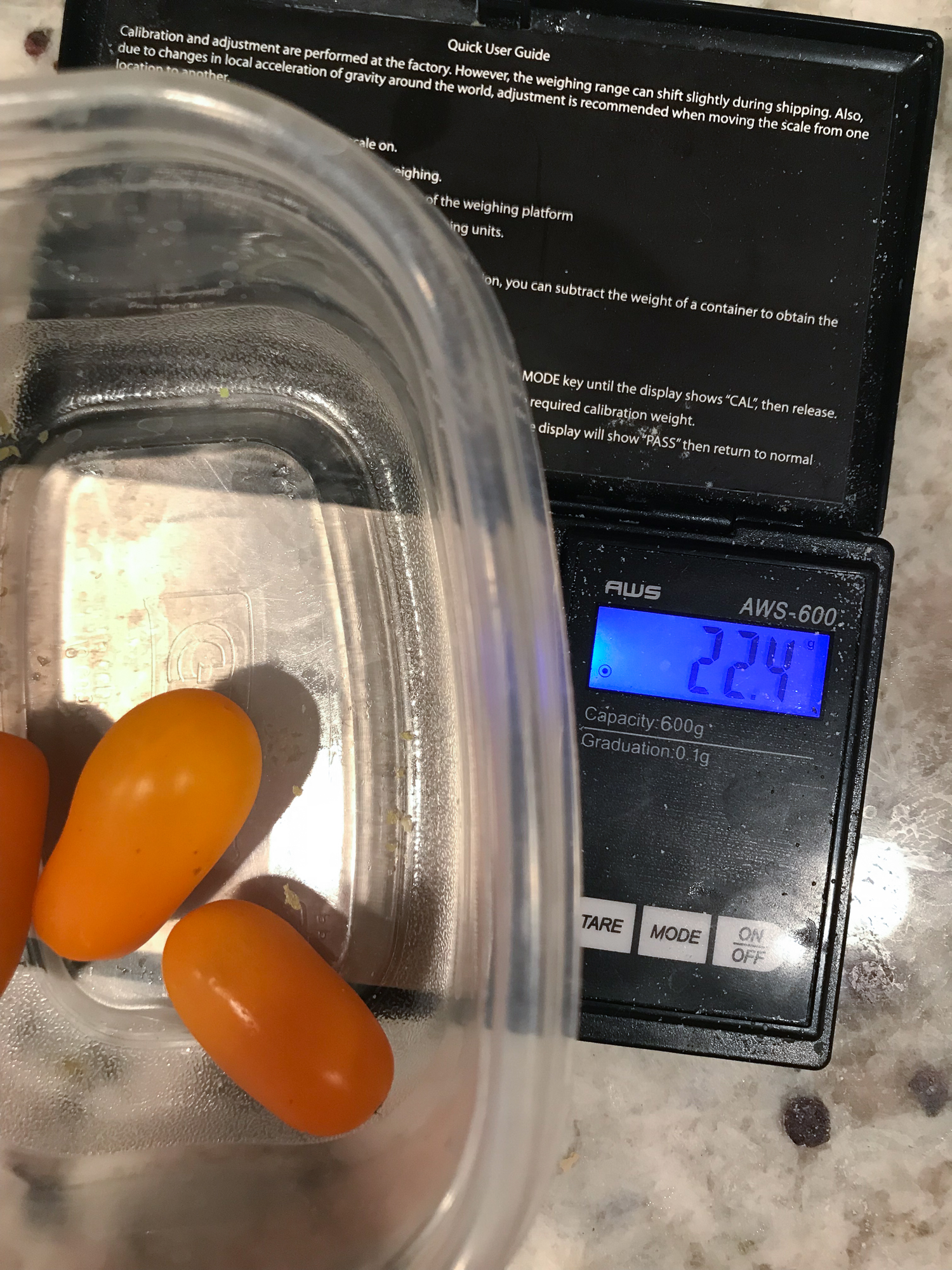
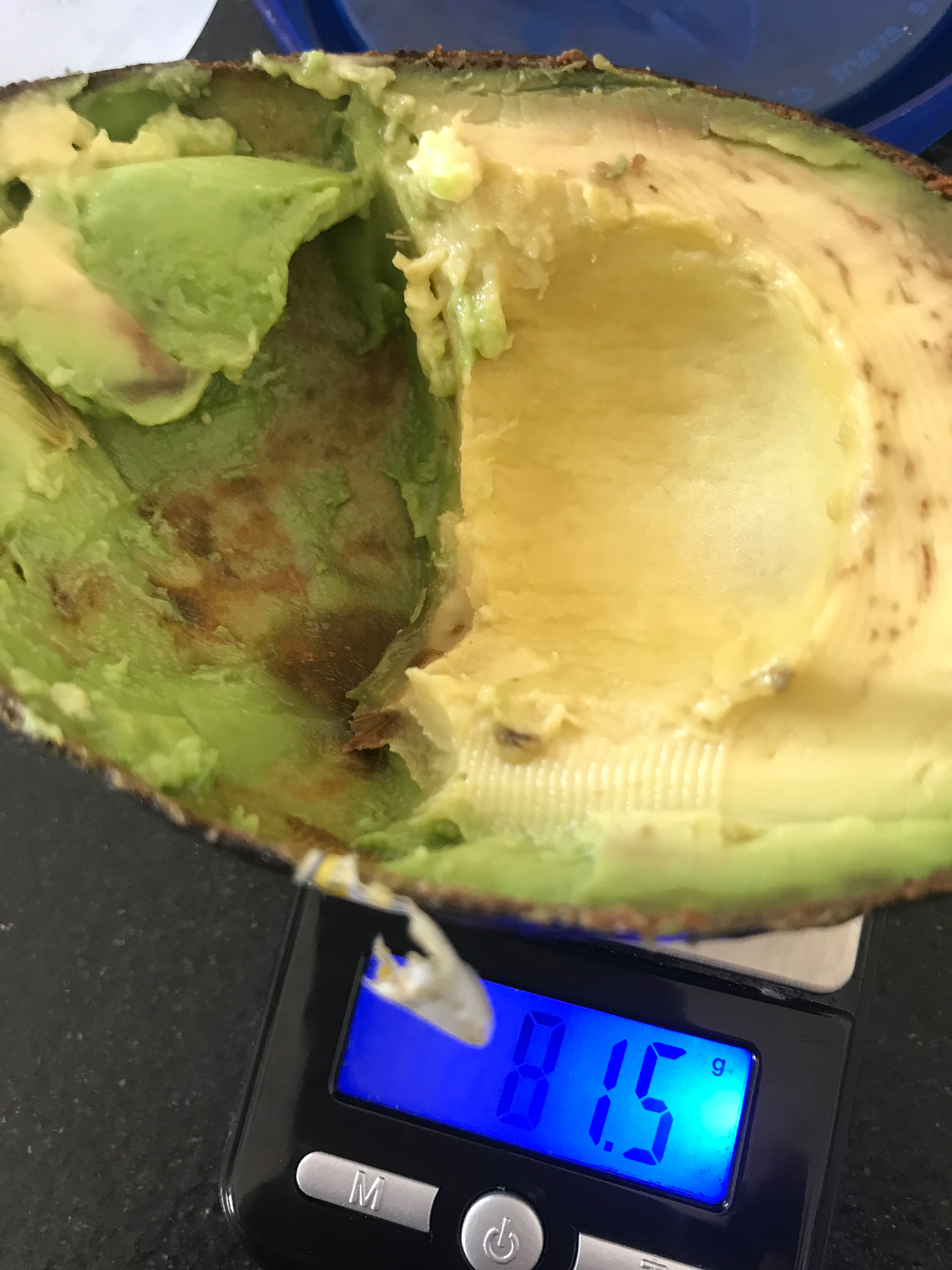
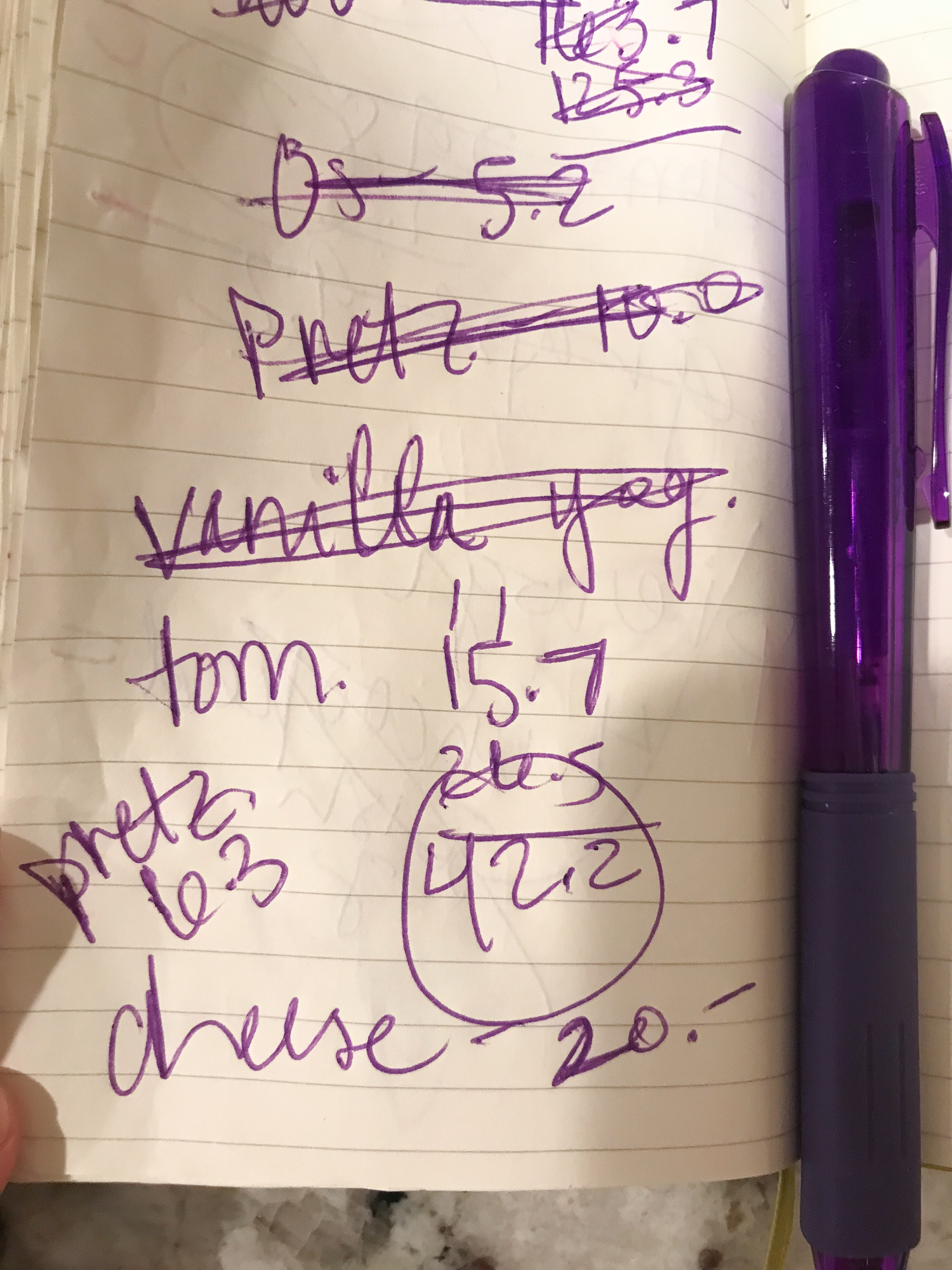
These days, we spend a lot of time every single day managing Vera’s PKU. We spend a lot of time at Rady Children’s Hospital, too. Weekly blood work. Appointments with Holly our dietician and metabolic specialists. We are working on getting her Phe levels within a specific range that is best for her brain and body. We must weigh everything Vera eats and drinks. And if she doesn’t eat or drink it all, we then weigh the remains, subtract and log the numbers into an app that keeps track of it all. She also has to drink a special medical food formula 3 times a day and will have to for life (that’s what’s in all of those bottle pics below). We have a little notebook on the kitchen counter where we take quick notes when we don’t have time right then and there to enter the numbers into the app. Well, enough time or if we feel like we’ve been on our phones too much already logging “the numbers” and we want to give our girl our undivided attention. At the end of the day, if we are high or low on Phe, we calculate a dinner that makes up wherever her numbers are lacking.
But our goal number is ever-changing, depending on growth spurts, illness, a shift of the wind (only kidding, but sometimes I’m not quite sure), etc. One of the first things Vera’s doctor told us at the metabolic clinic was, “You’re going to feel like you’re always chasing your tail,” with PKU. And admittedly, some days definitely feel that way. We have to be flexible. Always prepared with low, middle and high-ish (for Vera, at least) Phe foods. And be okay not achieving her perfect range every single week even though we’re technically doing everything right to do so. Hmmm. Funny how God keeps nudging me further and further away from being in control.
Poor girl can never ever ever have bacon this side of heaven. (Yes, there is bacon in heaven.) No meat. No eggs. No dairy. No nuts. No (regular) bread or rice or pasta. I remember laughing out loud to God when we heard the words “low protein.” Jesse and I had just started the keto diet. Aka: PROTEIN and fat. We’re also fans of eating Paleo, you know…PROTEIN. “You’re so funny, God.” I also thought it was pretty hilarious that we’d have to spend a lot of time in the kitchen. Like, every day. I’m not exactly a spend a lot of time in the kitchen kind of girl. At least I wasn’t before.
But, here we are, me in the kitchen. Our brave girl getting weekly blood draws, fighting the affects of high and low numbers fluctuating. But, I think that’s the easy part. The hardest part is not being able to use food as a tool for bonding and including her as much as we’d like to. We try to always have something on our plates that she can eat, but even then she can’t just take a bite. We have to get the scale out, weigh the food we’re sharing and log it. Subtract what she doesn’t eat. Do the math to determine what’s in the menu the rest of the day.
We do our best to eat a lot of snacks together: cucumbers, tomatoes, (she loves!) pickles. I eat more potatoes than I should, but, I’m only doing it for my daughter 😉 She can have (a calculated amount of) Chick-fil-A french fries, so yes, she’s still living a good life. We make her special low-protein rice and Jesse and I eat regular rice. We’re all getting the hang of it, even Vera. One day when she was “cooking,” before she gave Jesse some food, she first pretended to weigh it and then gave it to him to eat. Our girl is going to be okay.
The diet part is time consuming and sometimes tricky, but we’re all in because that’s what’s best for Vera. This isn’t just a special diet. Not to sound too dramatic, but the truth is, this is about her brain. And behavior. And sleep. And everything, really. Her PKU affects her overall health and well-being. And of course, as her parents, we want her to be as healthy and happy as possible.
This is a lifelong disorder. No, she won’t/can’t grow out of it. She’ll need to learn everything we’re doing for her and as she gets older, start doing some of these things herself.
Yes, there is a new-ish prescription drug that sometimes enables people with PKU to consume more Phe/protein. We don’t know yet if she’s eligible to take this medication. And, even if she is, it might not change anything for her.
“High-risk child.”
That international adoption doctor couldn’t tell us for sure how severe the effects PKU had already had on Vera. He couldn’t encourage us that, “Oh, she’s walking and talking, PKU’s got nothing on this girl!” Instead, on the other side of the phone, he hesitated and I could practically hear him shaking his head back and forth in uncertainty. And we aren’t naive. Jesse and I understand the full scope of this. There will be challenges. There already have been. She might have delays and learning disabilities. But, she can also have (and already is having!) an incredible, beautiful life, either way. And we can’t believe we get to be the privileged ones to experience it with her.
There are about 16,500 people living with PKU in the United States. More stats, facts and info here.
In case you’re curious about what Vera can and does eat, here are the staples we pretty much always have at our house…






























This Post Has 5 Comments
I am so grateful that God put Vera in YOUR life. Yes there will be challenges but there is no doubt that you and Jesse will face them and move on. I am praying that if the new medication is right for Vera then you will get it. In the meantime enJOY your daughter. This was definitely a match made in Heaven!🧡
Thank you so much for sharing in depth about your family’s journey with PKU. You and Jesse are amazing parents! My 17 month old daughter has some developmental delays and receives physical and occupational therapy every week, and just started speech therapy. There are specific steps regarding food and helping her to progress with eating solid food, and it’s a challenge for me sometimes to truly trust God in the process. I love that Vera can have CFA fries (my family frequents CFA). Do I spy cereal O’s as well? I didn’t see bananas on the list, but see a photo with Vera eating a banana. What kind of frozen yogurt (?) is she able to have? Do you buy the Plum Organics pouches in bulk, and if so from where?
Wow! What an amazing commitment you have both taken on. But well worth it I’m sure. Given the amount of lovely smiles from sweet V. Just a quick question, seeing you have to weigh all the foods etc is there a way to check if you’re doing it right? ie a blood test? Or mood swings? How do you know what you are doing is working?
My son is anaphylactic to peanuts and before going to parties, we’d feed him at home to ensure he doesn’t feel hungry or want to snack at the party.
The same goes for birthday parties at school. We had special things for him to eat instead (the teacher kept them)
So, I do understand a bit of your challenges.
But your commitment takes the cake.
Congrats on your beautiful girl 🙂
So curious about this. How was she diagnosed? Just a run of the mill blood test? What happens if she accidentally consumes a protein food? Is it like an allergy where there is a emergency solution? So happy she has diligent parents like you to give her top notch care. Thank you for sharing this story
Thanks, Bets! Yes, it’s a blood test. Newborns in the States are screened. We’re so grateful Vera’s orphanage had those screening capabilities. It’s not like an allergic reaction, but it is bad for her brain if her numbers are out of whack over a period of time. So, we have to keep an eye on her numbers by doing a blood spot at home every couple of weeks.